Physical Therapists aim to utilize clinical objective tests to confirm their evolving hypotheses on the source of patient’s current symptoms. One of the most beneficial areas of our Physical Therapy and orthopedic research has involved the confirmation or refute of known clinical tests to identify patients with or without a given diagnosis such as an ACL tear or SI joint dysfunction. Unfortunately, some areas of practice are too engrained with clinician bias, financial incentive (continuing education courses) or lack of research knowledge to evolve with current best practice patterns. One of the best examples of Physical Therapy practice refusing to change is the clinical “diagnosis” of SI joint dysfunction or pain based off the static palpation of pelvic bony landmarks or movement testing of this joint. Despite an low average incidence of 13% in low back pain patients we are left to question how many patients have been incorrectly identified using these tests.
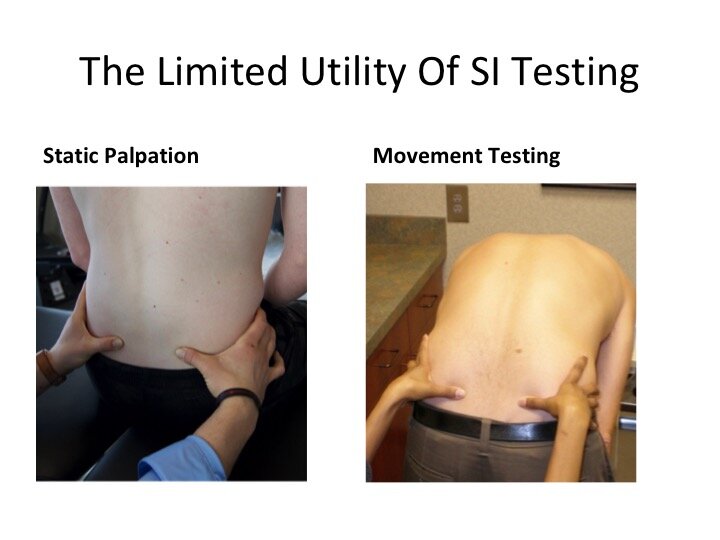
In a previous blog we discussed the limitations of these tests and best practices, provocative testing, for the confirmation of a SI diagnosis. While the provocative testing clusters by authors including Laslett and Van der Wurff represent current best practice for the clinical diagnosis of SI pain, static palpation and dynamic movement tests are still utilized by clinicians. These two categories of testing are wrought with error and their reliability and validity often fall below the coin flip level of 50%. Since the 1980s we have known agreement on the palpation of landmarks such as the ASIS, PSIS, and iliac crest fall below 50% on reliability between testers. This is surprisingly bad when you consider clinicians were offered either two (high or low) or three choices (high, low, or level). In turn, since the 1980s motion testing including the standing flexion, seated flexion, long sit or yo yo test, and prone knee test also have fallen below 50% on tester reliability. Additional studies have shown clinicians at times even have difficulty agreeing with themselves on static and dynamic testing. In the 1990s authors began to question the validity of these tests for identifying or ruling out the presence of SI joint pain and have consistently found poor diagnostic utility of these tests.
As the old quote states, old habits die hard, and this is true with clinicians’ utilization of SI static and dynamic tests. Clinicians are encouraged to follow best practice patterns involving the provocative test clusters of the SI joint. Importantly, patients are encouraged to advocate for themselves on the limited utility of these tests to guide treatment decisions for pelvic or low back pain.