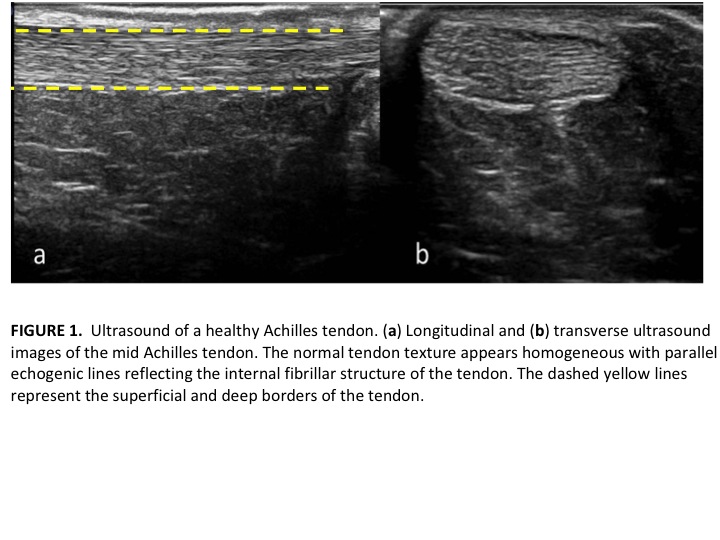
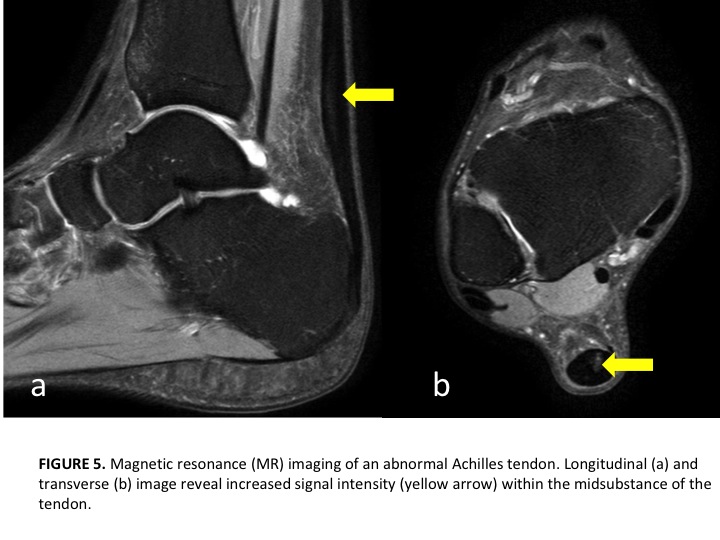
Our prior posts on tendon injuries have described the structural changes that take place with chronic symptomatic tendinopathies. The disorganization of tendon fibers and the body’s attempts to heal the injured tendon are best viewed on ultrasound or MRI imaging. MRI is a very sensitive tool, but lacks specificity meaning a positive finding may or may not be contributing to a patient’s presentation and symptoms. Further, we often see positive findings in asymptomatic individuals. Rio et al. described the presence of positive findings (tendinosis) in asymptomatic and active individuals and also the lack of impact of some findings on a patient’s presentation (Sports Med. 2014). The MRI and ultrasound images document both normal and abnormal imaging findings. Images courtesy of Docking et al. JOSPT. 2015.
In the pictures above, we can observe healthy tendon alignment primarily in parallel to resist and absorb tensile forces across the ankle joint, as well as, a high water and protein content reducing friction through the tendon. Conversely, a tendon with features of tendinosis demonstrates a disorganized tendon structure where tendon cells (tenocytes) are in higher numbers and have a more rounded appearance. This appearance makes the tendon less resisted to traditional tensile forces since the tendon is not arranged in a parallel alignment. Finally, there is an ingrowth of nerve fibers and blood vessels which likely contribute to the increased pain and symptoms noted in the achilles as well as in other structures within the body (central sensitization). If a tendinosis progresses in nature, partial tears in the tendon can also be noted on MRI. The accuracy of these changes on MRI explaining a patient’s symptoms is described as diagnostic utility.
MRI and ultrasounds greatest limitation on accuracy may be the lack of agreed upon gold standard in the literature. In a review of the literature Docking et al. reports the specificity for diagnosis with MRI (.68-.70) and ultrasound (.63-.83) for tendinopathies. Up to 59% of asymptomatic individuals will document some change within the tendon on imaging. These numbers show a degree of false positives making the clinical examination an essential part of any clinical diagnosis. This is consistent with the majority of musculoskeletal problems. If we rely solely on the MRI findings we run the risk of being incorrect in both our diagnosis and treatment. This will lead to higher healthcare costs and a longer duration of care for the patient.
In short, imaging can be a helpful component of our clinical diagnosis but only if we can use our subjective and objective examination to distinguish between asymptomatic tendinosis or symptomatic tendinopathy. In addition, an image rarely is helpful in determining how to use manual therapy and exercise to appropriately treat the patient.