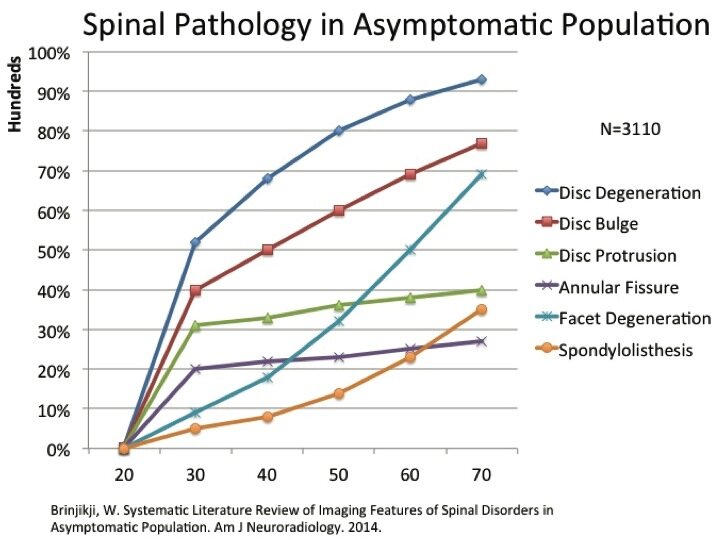
Degenerative Disc Disease (DDD) is a commonly utilized “diagnostic” term given to patients frequently after neck and low back MRIs. It is hard to think of a more uninformed and harmful diagnosis in musculoskeletal medicine than DDD. Initially utilized to describe age related changes in the spinal structures secondary to aging, DDD continues to induce fear, anxiety, and lowers self efficacy in patients with neck and low back pain. As an aside, we fret much less about the degeneration of our skin (wrinkles) or hair (thin, loose, and grey). Most striking is how common this diagnosis is among pain free patients on MRI scans (see graph above). After age 30, approximately 50% of asymptomatic patients will be diagnosed with DDD with close to 90% being diagnosed by age 60. This diagnosis has led to countless dollars being spent on unnecessary procedures including office visits, medications, injections, and surgery. If this term and diagnosis has done anything it has perpetuated the problem of over medicalization and harm in patients with spinal pain.
This is not to say DDD cannot be a painful condition, but spinal pain is often incorrectly, oversimplified to a single structure in the spine (disc, ligament, arthritis, etc.) Pain is a complex process involving multiple systems in the body from our tissues to our brain. Current pain science research highlights why some individuals may be more susceptible to spinal diagnoses than others. Similar pathologies in the spine such as disc herniations, degeneration, and arthritis frequently present differently based on individual patient factors. In short, an individual’s MRI findings provide part but not all of the answers behind their symptoms.
An individual’s emotional, mental, and physical health often act as important mediators between spinal pathology and expression of symptoms. For example, patient’s with adequate or superior strength for their chosen activities will generally express less pain than a weaker peer. In addition, a patient with greater self efficacy and confidence will also express fewer symptoms than a more fearful peer with lower levels of self efficacy. These are just a couple examples and a review of the pain literature is not the intent of this post. Instead practitioners in health care system treating spinal pain should strive to provide more accurate assessments of a patient’s spinal pain instead of relying solely on diagnostic imaging. The old saying, “the difference between pathology and pain is the patient”, rings true. At a minimum, we can help patients interpret their diagnostic imaging in relation to their age matched peers. At times the only abnormal scan is to have a negative or normal spinal MRI scan.