A recent clinical practice guideline was published advising clinicians and patients on the management of achilles tendon injury (tendinopathy). These guidelines are based on both the available medical research and medical opinions from experts in the field. The Journal of Orthopedic and Sports Physical Therapy reported the following for management of mid portion achilles tendinopathy (Martin et al. 2018).
Grade A – Strong Evidence
Exercise – Exercise utilizes progressive loading of the injured tendon and promotes tendon healing or remodeling. This process occurs through mechanotransduction and creates a stronger, healthier, and more resilient achilles tendon. Evidence supports the use of both eccentric exercise or a heavy load concentric and eccentric exercise prescription. Conversely, complete rest is not recommended due to its’ negative effects on the healing process.
Grade B – Moderate Evidence
Activity Modification – As we stated above, complete rest of an injured tendon often leads to delayed or incomplete healing of the injured tissue. A tendon has limited blood supply and metabolism compared to other body tissues requiring exercise to facilitate the healing process. A progressive, goldilocks approach is recommended because doing too little is just as harmful as doing too much. As your tissue heals and becomes resilient to a certain level of activity, the load and exercise volume is increased slowly to promote further healing in the tendon. This process is continued until you return to 100%. Injured tendons can take up to 1 year to completely heal at the tissue level and patients are advised to continue to exercise even after resolution of their symptoms, usually around 12-16 weeks.
Grade C – Weak Evidence
A lack of ankle bending or dorsiflexion is a commonly found risk factor and corresponding impairment in patients with achilles tendinopathy. Stretching of the calf and plantar flexors is commonly prescribed in patients with tendinopathy but the supporting evidence for this stretching is weak. We commonly recommend utilizing strength training within the ankle’s available range of motion instead of static stretching. Recent evidence suggests eccentric strengthening is equally effective to static stretching for mobility.
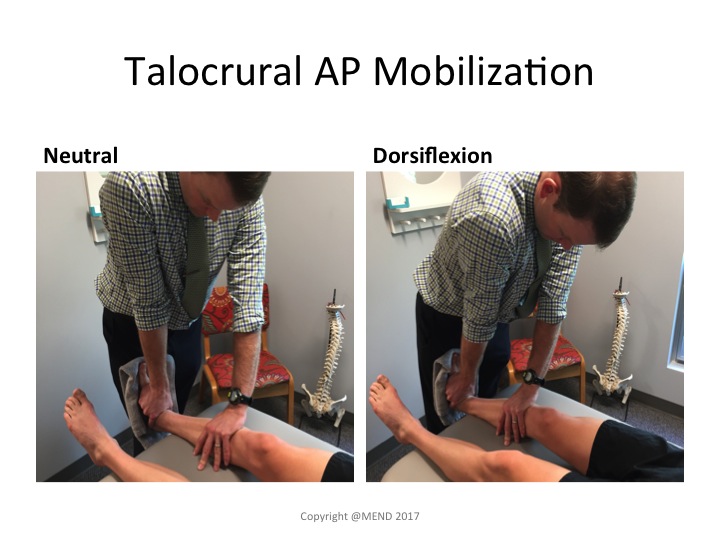
Further research is needed regarding other commonly utilized achilles tendinopathy including manual therapy. In our Boulder Physical Therapy practice we find the utilization of joint manipulation, mobilization, and dry needling to be very effective in the short term for reducing pain and improving patient function. These passive interventions are quickly withdrawn as patient’s begin to load their injured achilles tendon tissue.
Conflicting evidence was found for utilization of heels lifts or orthotics in the management of this condition. We do not recommend these inserts in our practice due to their short term, limited effectiveness and potential for creating long term problems including joint tightness and muscle weakness.