As more research about the novel coronavirus COVID-19 is developed, it is important to consider the effects of the disease on the pelvic floor and associated body systems and functions. The implications are both direct, i.e. affecting the cells of the bladder and small intestine, and indirect by disrupting function in the pulmonary system, in particular the diaphragm, which is an integral part of pelvic floor function.
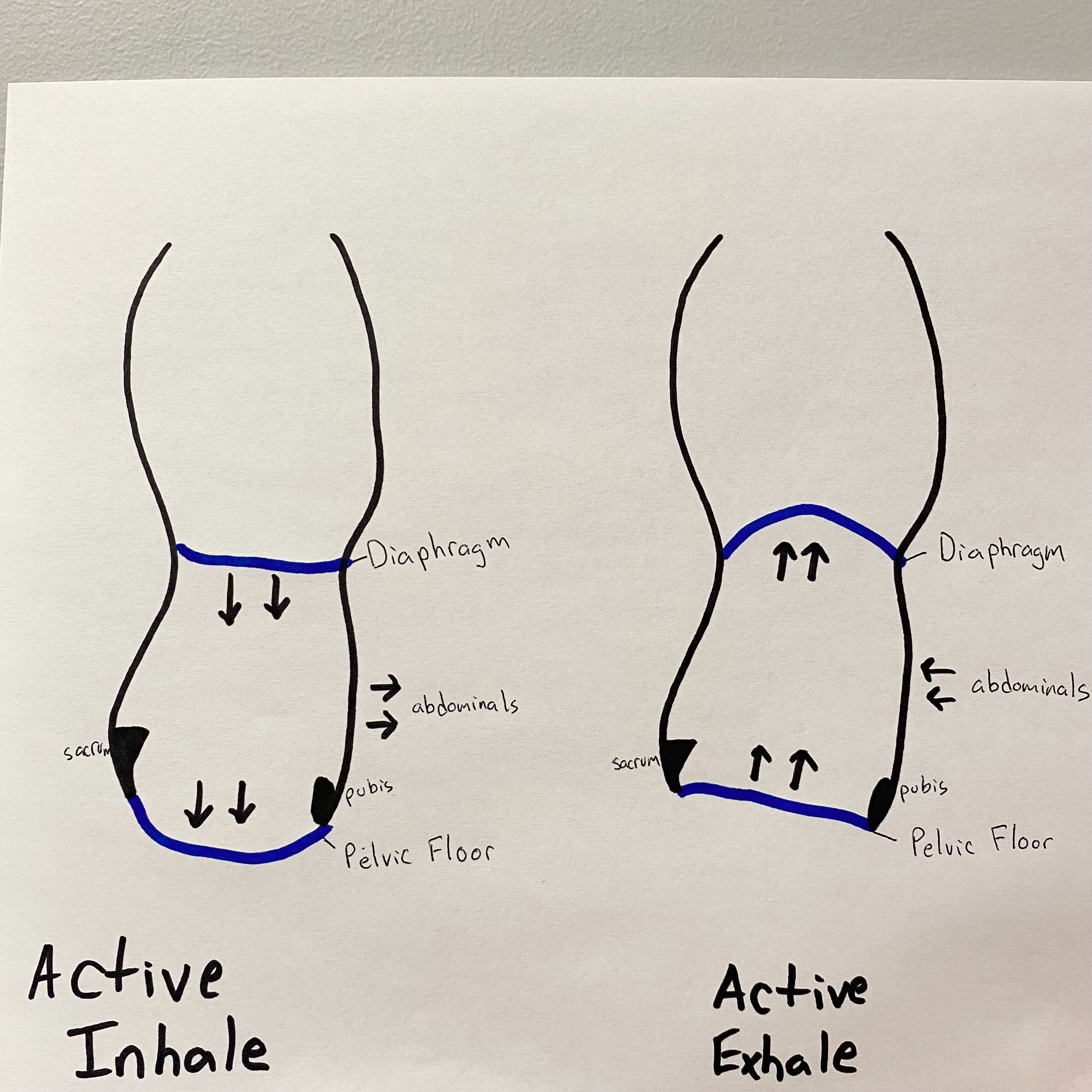
Think of the pelvic floor muscles and the diaphragm as a piston that is continuously working together with each breath we take. Visually, picture the diaphragm as the top of a soda can while the pelvic floor muscles are the bottom of the can. During inhalation, the diaphragm contracts downward in order to allow air to fill up our lungs; in response, the pelvic floor muscles lengthen towards our toes to accommodate the increased pressure in our abdomen. Once we exhale, the diaphragm recoils back up into its resting position and the pelvic floor muscles also rebound upwards. When one of the pieces of this system is dysfunctional, there is a subsequent effect on the other. We utilize this system for management of intraabdominal pressure which in turn can affect bladder, bowel, and gastrointestinal function as well as contribute to abdominal and pelvic pain.
Direct Implications of COVID on Functions of the Pelvic Floor
COVID-19 virus attaches to host cells by binding to ACE2 receptors. In addition to our respiratory tract, ACE2 receptors exist in our kidneys, bladder, and ilium. It is well documented that the coronavirus attacks the host via binding to cells in the pulmonary system, bladder, and ileum (the most distal part of the small intestine). Once infected, the immune system cascades into an inflammatory response which damages not only the virus, but has potential to damage the healthy host cells as well. This can lead to dysfunctions in the urinary and bowel systems even after a person has recovered from COVID. Additionally, there is research showing connections between COVID and the reproductive system of both men and women. Increased cases of erectile dysfunction have been found in those who have had COVID due to the virus targeting Leydig cells within the testicles. In women, connections have been made between estrogen and COVID, showing higher levels of estrogen may have a protective effect against COVID. So the virus itself has the capability of impacting all three major body systems regulated by the pelvic floor: the urinary, gastrointestinal, and reproductive systems.
Indirect Implication of COVID on the Function of the Pelvic Floor Musculature
With COVID, normal breathing physiology (described above and shown in the picture below) can get thrown off in a few ways. When we cough, it places an excess of pressure through this system and if the pelvic floor is underactive, or not strong enough, it cannot withstand that quick pressure increase and the result can be leakage of urine. We call this leakage of urine with coughing stress incontinence. In research conducted on patients with chronic coughing, these individuals demonstrate higher incidence of urinary incontinence, fecal incontinence, and pelvic organ prolapse due to chronic fatigue and under activity of the pelvic floor muscles. This stress incontinence can linger even after COVID is resolved.
COVID can also affect this system in almost the opposite way. Instead of repetitive bouts of pressure from coughing, some people will experience restricted breathing and restricted lungs from COVID. These people will not be able to take deep and large breaths and likely will result in taking small frequent chest breaths. With less movement in the diaphragm, the pelvic floor will have less movement as well. This can result in or exacerbate what we call an overactive pelvic floor. An overactive pelvic floor includes muscles that have difficulty relaxing out of the tension they hold and presents with symptoms of pelvic pain, constipation, pain with intercourse, and also incontinence. Further, difficulty breathing upregulates the sympathetic nervous system (i.e. the flight or fight response) which causes increased urinary urgency, a symptom of an overactive pelvic floor. Again, these symptoms may linger even after COVID is resolved.
Other considerations for more serious cases of COVID include: long hospital stays leading to deconditioning of the pelvic floor, catheter use, and ventilator use. Those on a ventilator for 6 or more days are at a two fold risk for developing constipation.
Thus we can conclude the answer to the main question of this blog is yes – patients suffering from residual COVID-19 symptoms may also see new onset or worsening pelvic floor symptoms. Once a patient has been diagnosed with COVID-19 and/or “long haul” side effects, it is imperative to discuss these symptoms to ensure proper care is received. Some symptoms may seem to be unrelated, but as more knowledge is gained on the direct and indirect effects of the virus, it is obvious there is correlation to pelvic floor dysfunction. A pelvic floor physical therapist can assess the function of the pelvic floor, abdominal, and respiratory muscles, as well as the urinary, bowel, and GI systems to determine the correct course of treatment and education to restore normal function and negate long-term effects.
Click Here to schedule with a pelvic health specialist at MEND physical therapy in Boulder today!
Siracusa, Carina PT, DPT; Gray, Amelia PT, DPT Pelvic Floor Considerations in COVID-19, Journal of Women’s Health Physical Therapy: October/December 2020 – Volume 44 – Issue 4 – p 144-151
Hsieh TC, Edwards NC, Bhattacharyya SK, Nitschelm KD, Burnett AL. The Epidemic of COVID-19-Related Erectile Dysfunction: A Scoping Review and Health Care Perspective [published online ahead of print, 2021 Sep 20]. Sex Med Rev. 2021;S2050-0521(21)00077-9.
Costeira R, Lee KA, Murray B, Christiansen C, Castillo-Fernandez J, Ni Lochlainn M, Capdevila Pujol J, Macfarlane H, Kenny LC, Buchan I, Wolf J, Rymer J, Ourselin S, Steves CJ, Spector TD, Newson LR, Bell JT. Estrogen and COVID-19 symptoms: Associations in women from the COVID Symptom Study. PLoS One. 2021 Sep 10;16(9)