The Ironic Reality of Injury
As a physical therapist, I help people move better, recover from injuries, and return to doing what they love. But despite my knowledge and training, I’ve dealt with a long history of injuries myself. It’s a humbling reminder: no one is immune to the physical demands of sports— especially when injuries are left untreated. Physical therapy didn’t just heal my body—it taught me how to move and think differently.
What I’ve learned is this: our bodies are incredibly adaptive. One injury can start a domino effect that changes the way we move, leading to pain, dysfunction, and compensation patterns that show up years later. And the most overlooked piece in that puzzle? Breathing.
Where It All Began
My injury story began at 13 on the tennis court, where a sharp pop in my right shoulder led to a dislocation. At the time, I didn’t realize that this single injury would set off a chain reaction: compensating for my right shoulder forced me to land on my left ankle repeatedly, leading to ankle sprains. Like many young athletes, I kept pushing through, unaware that one injury was quietly fueling the next.
Missed Opportunities in High School
Throughout high school, my right shoulder dislocated multiple times—during basketball, track, and tennis. In my sophomore year, my mom and I went to one physical therapy session, but we didn’t follow through. Looking back, I wish that physical therapist had emphasized the importance of strengthening my rotator cuff and sticking to a consistent plan of care. Instead, they let me believe that surgery was still an option, but I never took any action. I certainly didn’t realize that early physical therapy could’ve changed everything.
Learning to Breathe—Literally
During my freshman year, I was a natural sprinter, competing in the 100m, long jump, and triple jump. One day, after a tough track practice with sprint intervals, I felt an unfamiliar sensation—my throat and chest felt tight, and I was gasping for air. Later, I was diagnosed with exercise-induced asthma (technically “vocal cord dysfunction”). No one ever taught me how to breathe—not just with my lungs, but with my diaphragm, core, and pelvic floor.
I relied on my inhaler for much of my early athletic career, fighting for air during intense workouts, which made me hesitant to push myself. I didn’t yet understand how crucial breath control was—not just for performance, but for stability and recovery.
College: More Sports, More Injuries
College brought more injuries. I played on a competitive club tennis team, where I continued to experience right shoulder dislocations and left ankle sprains. One day, while sprinting for a ball, I sustained my first serious left knee injury. I partially tore my MCL and somehow sustained a patellar avulsion fracture. At the time, I didn’t have a physical therapist advocating for me, and I was left managing my symptoms on my own once again.
The most telling sign that my body was out of balance? The injuries began migrating to the right side—right foot plantar fasciitis, right knee pain, right hip tightness, and eventually, lower back pain. I was entering a vicious cycle of chronic injuries, and it became discouraging.
Discovering CrossFit (and My Limits)
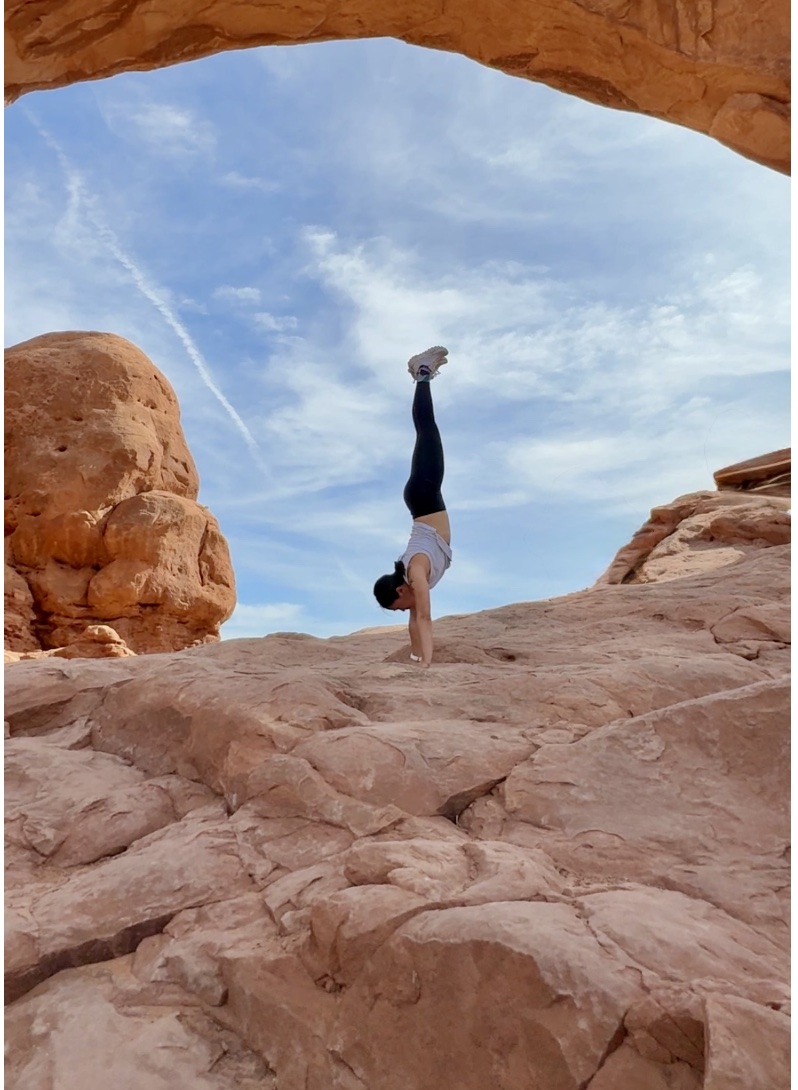
While attending physical therapy school in Arizona, I burned out of tennis and discovered CrossFit. It was an intimidating sport, but with encouragement from a classmate, I decided to give it a try. After the first workout, I “drank the Kool-Aid”. The dynamic movements— handstand push-ups, toes-to-bar, muscle-ups, wall balls, clean and jerks, snatches, and SkiErg— captivated me. At first, RX workouts felt nearly impossible, but I pushed myself to reach that standard.
I began to understand the demands of the WODs and the anatomy of aerobic and anaerobic programming. Whenever there was an endurance workout, it became clear that my breathing was the limiting factor in every workout. Running at sea level felt good, but back home in Colorado, I struggled. That’s when I realized something powerful—how and when I breathed directly affected how I moved.
The Breaking Point: Urinary Incontinence
As my fitness improved with CrossFit, I developed stress urinary incontinence— especially during double-unders, powerlifting, and running. What started in the CrossFit gym quickly started affecting my daily life—needing to rush to the restroom as soon as I got home, sneezing or feeling a sudden urge when stepping in the grocery store.
It wasn’t until after I graduated physical therapy school that I finally sought out pelvic health treatment. After just one session, I was able to run a mile without urgently needing to pee. I realized I had been coordinating my breathing and pelvic floor incorrectly for years. I began paying attention to my breath—not just during mid-workout, but recovery. This experience was eye-opening.
Once I learned how to properly coordinate my breath and core, my body felt calmer. I could finally focus on performance—not on my bladder. This is one of the many reasons I chose to integrate pelvic health into my physical therapy practice.
Less Is More: Redefining Fitness
I used to train six days a week, thinking more volume meant more results. Now, I work out three times a week—and I feel fitter, stronger, and faster than ever before. Why? Because I prioritize recovery. I listen to my body. I cross-train with yoga and breath work. I meditate. I spend more time tuning in and less time pushing through.
Yoga helped me regain mobility and resolve my hip tightness. Breath work helped me ditch the inhaler. And pelvic floor physical therapy? It changed my life.
When I competed in the 2019 CrossFit Open, I finished in the 46th percentile worldwide. This year, I placed in the 94th percentile. But the real victory? I haven’t dislocated my right shoulder in years. I feel stronger—not just in my body, but in my ability to trust it.
A Holistic Approach to Health
Today, I regularly see health professionals—massage therapists, acupuncturists, mental health therapists, and of course, physical therapists. Not because I’m broken, but because I know that proactive care matters.
I stay consistent with my own programming: breathing exercises, pelvic floor training, core stability, and foundational strength work for different body parts. These aren’t flashy—but they’re the building blocks that allow me to train harder and live relatively pain-free. I feel fortunate to understand how to modify exercises to suit my body’s needs, and you’ll often see me incorporate my physical therapy exercises into the WOD. What started as breathwork for my lungs has evolved into breathwork for my mind. I feel less anxious, more grounded, and more in tune with my body’s needs.
In CrossFit, I’ve learned to pace intensity with breath. In yoga, I’ve learned to connect breath to intention. Physical therapy gave me the body awareness to thrive in both.
What I Want You to Know
If you’re a young adult struggling with injuries from CrossFit or other sports—you’re not alone. You can move well again. And often, it starts with something as simple and overlooked as your breath.
Our bodies are resilient and intelligent—but they also need guidance, especially after injury. Pelvic floor physical therapy gave me back control, confidence, and performance I didn’t even know I was missing.
If I could go back in time, I’d start physical therapy sooner. I’d stick to the plan. I’d learn how to breathe, stabilize, and recover. But now I get to use that knowledge to help others heal— before the compensation patterns take hold.
Ready to Rebuild From the Core?
At MEND, I specialize in pelvic health and orthopedic for active individuals. If you’ve been struggling with persistent injuries, urinary incontinence, or feel like something just isn’t clicking—let’s talk. Healing isn’t just about getting rid of pain—it’s about understanding your body’s story and giving it the tools it needs to thrive.
Click HERE to schedule your next appointment with the experts at MEND